Presented by Providence Ventures.
Second in the series,”Strategic VC as a Secret Weapon in Healthcare.”
It’s no secret that healthcare transformation is a herculean endeavor. Last month, we highlighted Providence Ventures’ commitment to sourcing, funding, and closely partnering with companies who are helping drive that transformation by focusing on some of the biggest challenges in healthcare.
So what areas are most in need of innovative solutions? For us, patient-provider communication, consumer engagement, and chronic disease prevention represent some of the major problem spots that have our attention. Here’s a look at three of the companies in our portfolio that help us overcome these specific challenges, and how we’re working with them to drive healthcare transformation at Providence St. Joseph Health and across the industry.
Providing instant interpretation services: InDemand Interpreting
One in five U.S. residents doesn’t speak English at home. Of course, communication is critical to any medical encounter, so it’s not surprising that patients with limited English proficiency who don’t receive high-quality interpretation services are more likely to suffer adverse medical events, require longer hospital stays, and have higher readmission rates. Yet, in-person interpreters are difficult to scale across multiple facilities and language needs, and telephonic interpretation is impersonal.

Enter InDemand Interpreting, a Providence Ventures portfolio company that offers patients and clinicians immediate access to face-to face interpreters via point-of-care video connectivity.
Providence Ventures invested in InDemand in 2014; since then, our strategic relationship has matured significantly. Together, we identified additional expansion opportunities across our markets and supported the health system’s goal of streamlining multiple fragmented interpretation technologies. This collaborative business development work, in addition to
enabling continuous feedback on the platform from internal operating partners, led to system-wide standardization, which reduces costs and improves overall patient care.
InDemand’s growth is a testament to the need for solutions like this to better care for our under-served communities. The win-win outcome helps solve the increasingly pervasive challenge of delivering high quality healthcare to a growing number of patients with limited English proficiency, which aligns perfectly with Providence’s Promise to ease the way for patients in our communities.
Matching patients to providers: Kyruus
You probably wouldn’t frequent a retailer with an online catalog of old or outdated inventory. Or imagine shopping for a flight online with an airline result that repeatedly states, “Whoops, sorry, not sure if we fly there anymore.” Outside of healthcare, ensuring that your ‘inventory’ or ‘product availability’ is up to date would seem like a simple task. Yet, inside of healthcare systems, the complexity of provider networks and employed and affiliated provider contracts lends itself to the extremely difficult process of tracking and presenting accurate provider information in real time. And it’s one of the biggest sources of frustration for consumers looking online to find a provider.
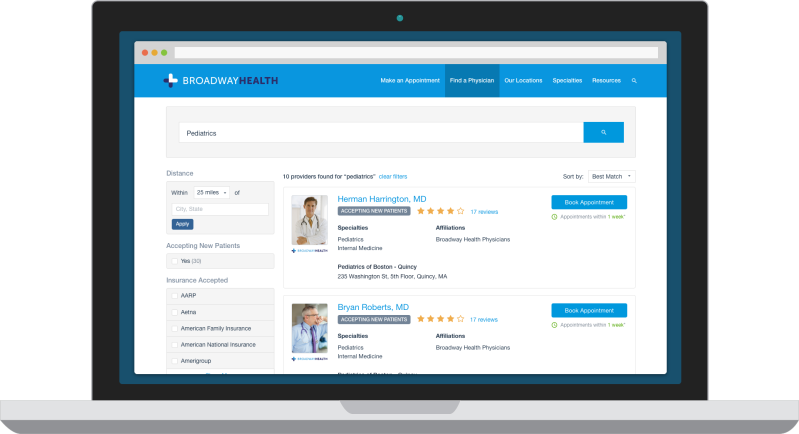
When Providence Ventures was formed in 2014, our health system was already working with Boston-based Kyruus to help solve this problem of matching patients to providers. Kyruus leverages a proprietary provider data management platform to enable health systems to put forth a better patient experience with provider search, match, and scheduling. We invested in Kyruus in the fall of 2015 in a round led by New Leaf Ventures that also included Leerink Capital Partners and McKesson Ventures — and our partnership has gone far beyond a typical commercial relationship.
Not only can Kyruus tap a stream of constant and in-depth feedback on the product from our operations leadership, but the company has also partnered with PSJH technical teams on the co-development of the consumer-facing platform. By working with Kyruus to ensure a more accurate provider directory as a foundation, Providence St. Joseph Health has been able to innovate on top of that, enabling more convenient access options and online scheduling capability for our patients. The Kyruus platform is now being rolled out system-wide. The technology can be seen here on the website for PSJH affiliate Swedish. This partnership is a great example of a health system working closely with a technology company to deliver the right solution needed to support both our patients and clinicians.
Preventing chronic disease: Omada Health
New data published in late 2015 revealed that half of U.S. adults are diabetic or pre-diabetic, adding up to more than 122M individuals impacted by this pervasive chronic disease. The enormous problem of obesity-related chronic disease is growing, and has been predicted to cost the U.S. over $300B by 2018 following the current trajectory. While the ability to prevent diabetes with intensive behavioral counseling programs has long been proven to work, reaching even a fraction of the patients at-risk for the disease has been nearly impossible with limited in-person programs.
Omada Health was the first company to digitize the clinically proven, but previously unscalable, Diabetes Prevention Program (DPP). Since the company’s commercial launch in 2012, it has become the nation’s largest provider of the DPP, having served over 120,000 participants to date.
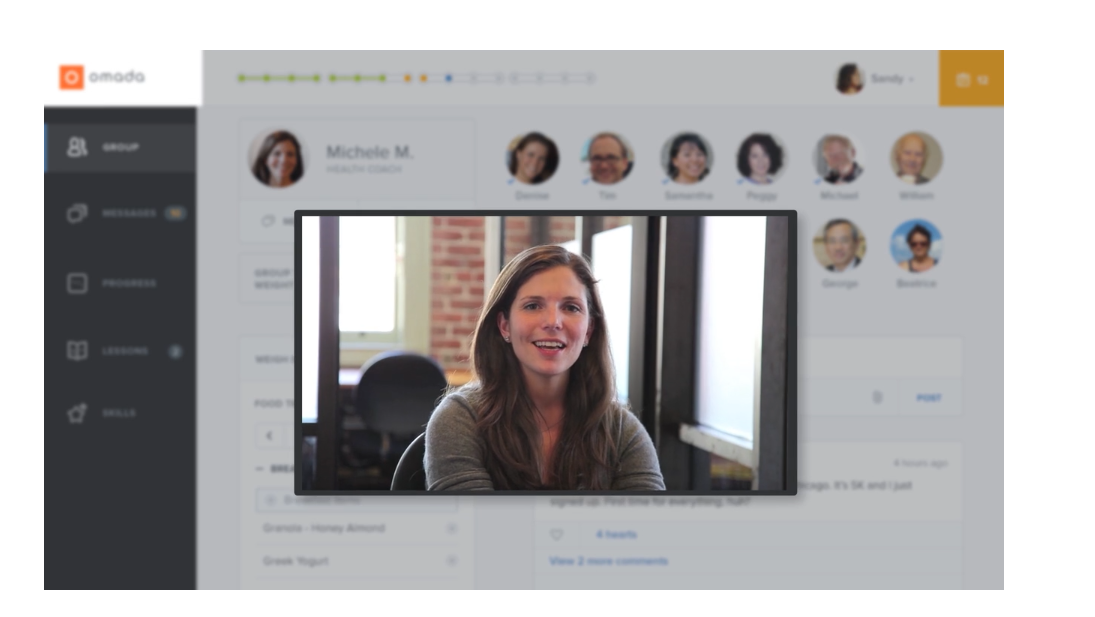
Interestingly, Omada’s initial introduction to Providence was not through clinicians and caregivers, but via Providence Ventures’ employee benefits leadership, who were seeking a program to help Providence employees get healthier. Self-insured employers have a critical interest in keeping their employees healthy as costs continue to rise and become an enormous financial burden on operating businesses.
After piloting the solution with over 1,300 employees who, on average, reduced their risk of developing diabetes by almost 40 percent, Providence was thrilled to expand the relationship with Omada, giving employees full access to the program as a preventative health benefit, as well as with an investment from Providence Ventures. Since then, Providence has deepened its relationship with the company through integration with the Providence Health Plan, participation in speaking engagements with our HR Benefits leaders, as well as collaborative projects on clinical referrals to the program. Importantly, Medicare will begin reimbursing for the DPP in 2018, which may serve as a much-needed catalyst to fueling collaboration between traditional healthcare providers and companies like Omada to provide scalable, digital therapeutics to the hundreds of millions of individuals in need. Omada recently closed another round of funding, led by a great partner to the company, health insurer Cigna.
In addition to the focus areas described above, there is a multitude of other healthcare problems that need to be solved. We’re constantly connecting with the leaders of our health system to better understand the complexities that drive those problems, and are actively seeking solutions from value-added technology platforms and tech-enabled services solutions. We’ll talk more about our perspective on some of those challenges and what our investment theses are in those areas in the weeks to come.
Sponsored posts are content produced by a company that is either paying for the post or has a business relationship with VentureBeat, and they’re always clearly marked. Content produced by our editorial team is never influenced by advertisers or sponsors in any way. For more information, contact sales@venturebeat.com.

